Welcome to the Pain Team webpage.
We understand that living with long-term pain or fatigue can be hard. It can affect your physical and mental health and stop you doing the activities you enjoy.
Our online programme can help you:
- Understand your pain and fatigue
- Learn ways to feel more in control
- Get back to doing the things that matter to you
What Will You Learn?
- What pain is and why it happens
- How to do your daily activities without making pain worse
- How to rest and move in a balanced way (this is called pacing)
- How to feel calmer and less stressed
- How to set small goals and celebrate your progress
Who Is It For?
This programme is for adults living with long-term pain (sometimes called chronic or persistent pain). You don’t need to be good at reading or writing. Everything is explained in a clear and easy way.
What You Can Expect
- Clear and simple information
- Tools to help you feel more confident
- A chance to learn what works best for your body
Remember
- You don’t need to do everything right away
- You don’t need to do it alone — ask for help if you need it
How to use the programme
The programme is split into different sections. Each section is under a different drop down heading below. It includes topics like:
- Pacing (how to save your energy)
- Sleep
- Managing flare-ups (when symptoms get worse)
- Mental health
Each part has:
- Easy-to-read information
- Videos and links to other helpful resources to explore
- Activities to try
- Ideas for using what you’ve learned in real life
You will learn more if you try the activities as well as read the information.
Don’t try to do everything at once. We suggest doing one section each week, but it’s okay to go at your own speed. You can also write down in a notebook how you feel and what helps you.
Our program is based on something called Acceptance and Commitment Therapy (ACT). This means it will help you make good choices, keep moving forward, and live a full life—even if you have pain. Before you begin the rest of the program, it will help to learn a bit more about ACT by reading the information below.
Acceptance and Commitment Therapy (ACT)
Some people with pain and fatigue feel there is no ‘medical’ treatment for their symptoms. They may believe they only have two choices: to give up or to fight the pain. But there’s another way. ACT (Acceptance and Commitment Therapy) is about living a meaningful life even with pain and fatigue. Fighting pain or fatigue can take a lot of energy and make things worse. Acceptance means being open to having pain, even if you don’t like it. It helps you stop struggling and focus on what’s really important to you—what brings joy and meaning to your life. Acceptance doesn’t mean you want the pain. It means you stop trying to control the things you can’t change and focus on the things you can change. There’s a saying that goes:
“Give me the courage to change what I can, the peace to accept what I can’t, and the wisdom to know the difference.”
You can watch a video that explains this more: Pain and Me: Tamar Pincus talks about chronic pain, acceptance and commitment
Values
Your values are the things that matter most to you. They help guide how you want to live and the kind of person you want to be. For example, being kind, honest, or helpful could be some of your values.
Sometimes, when people feel tired or unwell, they lose touch with their values. They might feel stuck or unhappy. But remembering what matters to you can help you make good choices and feel better.
Here are some values to think about. Which three are the most important to you?
|
Acceptance |
Curiosity |
Honesty |
Respect |
|
Adventure |
Encouragement |
Humour |
Responsibility |
|
Assertiveness |
Equality |
Humility |
Romance |
|
Authenticity |
Excitement |
Independence |
Self-care |
|
Beauty |
Fairness |
Intimacy |
Self-development |
|
Caring |
Fitness |
Justice |
Sensuality |
|
Challenge |
Flexibility |
Kindness |
Spirituality |
|
Compassion |
Friendliness |
Love |
Supportiveness |
|
Connection |
Forgiveness |
Order |
Add your own |
|
Contribution |
Fun |
Open-minded |
Add your own |
|
Courage |
Generosity |
Patience |
Add your own |
|
Creativity |
Gratitude |
Persistence |
Add your own |
If you lived your life based on what really matters to you:
- What would you do differently?
- How would you treat other people?
- How would you take care of yourself?
- What goals would you work on?
- What would you stop doing?
The worksheet below can help you think more about your values Values-Worksheets.pdf .
What’s the Difference Between Values and Goals?
- Values are about the direction you want your life to go. You never really "finish" a value.
- Goals are things you can work on and finish. These can relate to your values.
For example:
- Value: Being a loving parent
- Goal: Read a story to your child every night
- Value: Enjoying nature
- Goal: Take a walk in the park three times a week
Goal setting
A goal should be SMART:
- Specific – Know exactly what you want to do
- Measurable – Know how much or how often
- Achievable – Make sure it’s possible
- Realistic – Make sure it’s doable
- Time-limited – Set a time to finish it
Watch this video to learn more: Values vs Goals - By Dr. Russ Harris
Activity
Before you start the pain programme, take a little time to think about what’s important to you. What do you care about? What do you want to be able to do? What are your values and goals?
You could write these things down so you can look at them later.
As you go through the programme, try to think about how what you’re learning can help you reach your goals and do the things that matter most to you.
Pain is something we all experience at various points in life, and it is an important protective mechanism that actually keeps us safe from harm. Some people have pain that lasts a long time, and it can make life harder. About 30-50% of people have this kind of pain, and it can be tough to figure out what’s causing it or how to make it better. Pain can make it hard to go out, do your regular activities, or even just get through the day. Some people feel stuck in a "pain cycle," where the pain keeps affecting them.
But research shows that the more you understand pain and feel in control of it, the better you can handle it and feel better in the long run.

Types of Pain
There are two types of long-lasting pain:
- Primary pain: This kind of pain doesn’t always have an obvious cause. It’s often because the body’s nervous system (the system that controls your body’s reactions) gets too sensitive or overprotective.
- Secondary pain: This kind of pain comes from something that can be easily seen, like an injury or sickness.
Things like sleep, eating, exercise, and mental health can affect how much pain a person feels.
Understanding Pain and Your Nervous System
Pain is real, even if doctors can’t find a clear cause for it. Pain happens because of your nervous system, which includes:
- Your brain: It’s like a computer that makes decisions for your body, both big and small.
- Your spinal cord: A bundle of nerves that goes from your brain down your back.
- Your nerves: These are like cables that carry information from your body to your brain and back.
When you hurt yourself, your body sends a message to your brain to warn you. If the brain thinks something is dangerous, it will make you feel pain to stop you from making it worse.
For example, if you touch something hot:
- Your nerves feel the heat.
- The message goes to your brain.
- Your brain decides it’s dangerous.
- You feel pain and pull your hand away to stop getting burned.
Sometimes, pain can happen even if there isn’t damage. This happens because the body’s pain system can get too sensitive, like a loud alarm going off even when nothing’s wrong.
How Pain Can Be Tricky
Pain doesn’t always match up with what’s really happening in the body. Sometimes, pain can happen without an obvious cause, or it can feel different depending on things like the weather or where you are. People with long-lasting pain might have a nervous system that’s stuck in an “overprotective” mode, making everything feel like a danger.
How to Handle Pain
Understanding how your body works can help you handle pain better. There are things like sleep, exercise, eating well, and taking care of your mental health that can help reduce pain and improve your life.
Summary
Long-lasting pain is complicated and can affect many parts of life. Things like your body, your thoughts, and the world around you can all affect how much pain you feel. But by learning how to take care of yourself, you can manage the pain and still live a happy life.
Further Reading and Resources:
- Watch this quick video about pain: Understanding Pain: Brainman chooses
- Learn more about what happens in your body when you feel pain: Professor Lorimer Mosely, The Pain Revolution , April 2017
- Check out this website for more info about pain: Flippin' Pain
Living with chronic pain or tiredness can make normal activities, like going to work, taking care of others, shopping, and even hobbies, really tough. Some people also feel mentally or emotionally tired when trying to concentrate on tasks.
What is Pacing?
Pacing means managing how much you do to avoid making your pain or tiredness worse. It helps you take breaks or slow down to feel better. It includes not just physical rest but mental / emotional rest as well.
Boom and Bust Cycle
Sometimes when people push themselves too hard on a busy day, they end up feeling extra tired and in more pain afterward. This can make it harder to sleep, and then they might need to rest for several days. It’s easy to get stuck in a pattern of doing too much one day and then doing too little the next, which can make things worse over time.
Pacing an Activity
When you have chronic pain, doing something for too long can make your pain worse. It’s helpful to take breaks before the pain gets too bad. For example, instead of doing an activity for an hour, you could do it for 20 minutes, take a break, and then do a little more. This can help you feel better in the long run.
How Much to Do?
It’s hard to know how much to do. A good rule is to start small, like doing something for 10 minutes, then stop, even if you feel okay. If you feel fine after, you can try doing a little more the next time. If it makes your pain worse, try doing half of what you did before and slowly build back up.
The Phone Battery
Think of your energy like a phone battery. Some activities drain your energy fast, while others can recharge it. Activities that use lots of energy need planning to avoid completely draining your battery. It's important to make time for things that help you feel better as well.
|
Consider what activities or situations charge or drain your energy levels |
|
|
Things that CHARGE my battery
|
Things that DRAIN my battery |
Tools to Help You
There are tools, like special chairs or walking aids, that can make activities easier. These can help reduce strain on your body, and you can talk to a health professional to see what might work for you.
Spoon Theory
The Spoon Theory is a way to think about your energy. Imagine you have a certain number of spoons each day. Every activity uses up some of your spoons. If you have a busy day, you might run out of spoons, so it’s important to plan ahead and make sure you don’t do too much. Watch the video below to learn more about this.
https://www.youtube.com/watch?v=jn5IBsm49Rk
Barriers to Pacing
It’s hard to pace yourself sometimes because of family or work responsibilities, or because you feel frustrated or guilty. But it’s important to know that it’s okay to take breaks and not do everything all at once. Talking to others, like family or a therapist, can help.
Planning and Prioritizing
Planning ahead can help a lot. For example, if you know you have a busy day, leave extra time to take breaks. You can also prioritize tasks to do the most important things first and save others for another day.
Tracking Your Activity
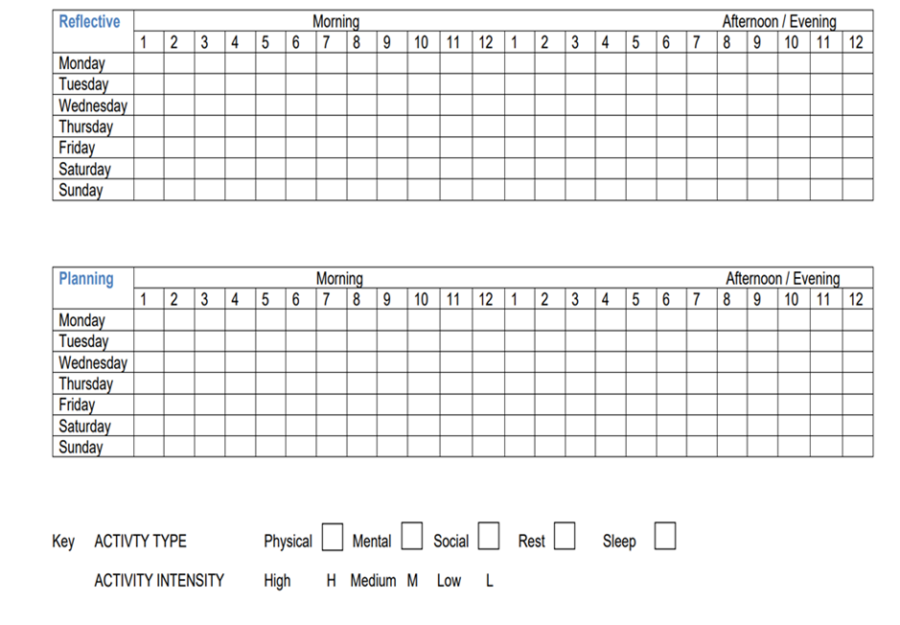
Keeping track of what you’re doing and how much can help you see where you need to slow down or take breaks. You can use an activity diary to keep track.
An activity diary helps you keep track of what you do each day and how your body feels. It’s like a journal that shows how you spend your energy throughout the day. This helps you learn how to balance your activities, so you don't do too much or too little.
How to Complete an Activity Diary
You will find an activity diary template at the bottom of the page. You can use this or make your own. Follow the steps below to complete the diary
1. · Date At the top of the page, write the date. This helps you remember what happened on each day.
2. · Time of Day Split your day into morning, afternoon and evening or record hourly like on our example.
3. What Did You Do? Write down the type of activity you did during each part of the day, for example, getting dressed, going to work, attending a meeting , meeting a friend. Remember activity can be physical, mental or emotional or social. Watching TV would be an example of rest.
4. How Did You Feel? You can categorise these activities as high, medium and low intensity depending on how much energy you need to spend. You can colour code them as given in the example. You can even write a word or draw a smiley face to remember how you felt about that activity. It can help to record your pain level at the end of each day.
Below is an example of a blank activity diary to complete or you can make your own.
Below is an example of a completed activity diary:
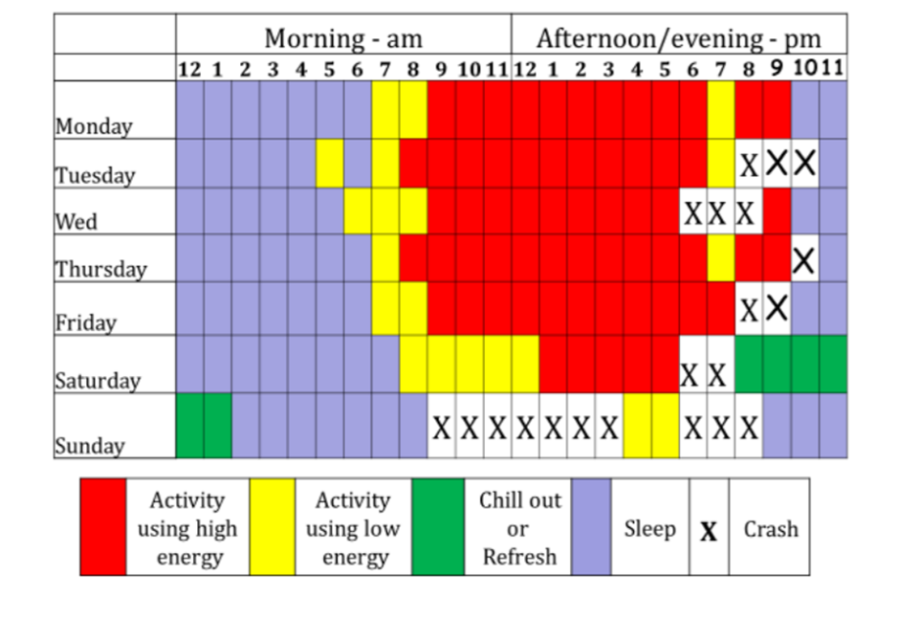
Try completing an activity diary like the one above for yourself for 2-3 weeks. Do you notice any patterns or anything you could change?
What did you learn?
At the end of the day, it can be helpful to write a note in your diary of one thing you learned e.g. I felt better when I took breaks, or I was sore after working too long.
It is important to notice early signs of pain or tiredness so you can take a break. Here are some signs to look out for: - Muscle tightness, slower movements, needing to rest more often, feeling more tired than usual.
Take a look at your completed activity diary and try answering the questions below.
- Are there any surprises?
- Are there any patterns or themes?
- Is there a balance between rest and activity?
- Do you spend most of your time on one particular type of activity?
- Which activity do you find most tiring?
- Is your day spent mostly resting? / Is there any rest during the day?
- How do you rest?
- Are your current activity levels working for you?
- If not, what might be more workable, what changes could you make?
Top Tips
- Celebrate small wins, like finishing one task or taking a break.
- Do harder tasks when you have the most energy.
- Write down what you do and how much to help you plan better.
Useful Links
You can find more tips and help on websites like:
Exercise and rest are both really important when you live with pain. They can help you feel better and make managing pain easier.
Exercise and Your Experience
If you’ve been active before, it can be hard to adjust your expectations when you have pain. You might try to do too much, and that can make your pain worse, which can be frustrating.
Sometimes, people like physiotherapists or personal trainers might not understand how hard certain activities are for you. When you can’t keep up with what others expect, it might make you feel bad about yourself or like you’re not doing enough. This can even make you want to skip the next appointment or exercise session.
There’s also a hidden effort involved in exercise. For example, swimming might seem like an easy exercise, but there’s a lot more to it than just going into the pool. You have to get to the pool, change, shower, dry off, and get home. For some people, swimming is a great exercise, but it might not be right for everyone.
When you have pain, exercise might stop being something fun and turn into something you do because you have to. But exercise can still be enjoyable if you find the right balance. If you finish exercising without making your pain worse, and you feel proud of yourself, that’s a big win!
You can learn more about exercising with pain in these two articles:
What is Exercise?
Exercise means doing physical activities with a purpose. Physiotherapists think about three kinds of exercise:
- Strengthening exercises: These help make muscles stronger.
- Cardio exercises: These make your heart beat faster and your lungs work harder.
- Flexibility exercises: These help you move your body more easily.
Most exercises mix all of these types together!
Why Exercise?
Exercise has many benefits, even if you’re not able to do the recommended amount each week. Doing a little bit of exercise is still better than doing none. Exercise helps calm down your nervous system and can make pain more manageable. Your body has a “comfort zone” for how much activity you’re used to. If you try an activity that’s too far outside your comfort zone, it might make your pain flare up. For example, gardening or painting might hurt because you don’t do them regularly enough.
Please find below more information on the benefits of exercise for general health which you can read about here:
https://www.nhs.uk/live-well/exercise/exercise-health-benefits/.
Or you can watch this video:
How to Exercise
It’s really important to find exercises you enjoy and ways to stay motivated. If you’re not sure where to start, you can talk to someone who specializes in exercise for people with pain, like a Rehabilitation and Exercise Practitioner (REP). Your physiotherapist can advise on this.
Thriving Nottingham can also help you get more active. They might help pay for gym or swimming sessions, connect you with local exercise groups, and give you one-to-one advice to keep you motivated. You can learn more and sign up by clicking here. Thriving Nottingham | Helping you to live well and feel great .
Any activity which gets you moving such as gardening or dancing can help – exercise is not just about the gym or sport. Social Prescribers can link you up with community groups that match your interests. You can ask your GP practice for more information on this.
Here are some exercise options to check out:
- Versus Arthritis – Exercising with Arthritis
- Stronger My Way
- Joint Pain Programme | Nuffield Health
- Dance 4 Fibromyalgia
- Hydrotherapy Pool
- Derby Back Care
You can learn more about other people’s experiences of exercising with chronic pain here: Paul and Anne discuss the benefits of Tai Chi with osteoarthritis
Rest
Getting good rest is just as important as exercise for your physical and mental health. Rest helps your body in many ways, like:
- Lowering your heart rate and blood pressure
- Reducing muscle tension
- Helping your digestive system work better
- Making you feel better emotionally and mentally
Resting doesn’t just mean sleeping. It can be physical, mental, and emotional rest. Sometimes, things like being on your phone, watching stressful TV shows, or doing other things that make you think a lot don’t actually count as rest. People find different things restful, like spending time outside, taking a warm bath, or listening to calming music.
Mindfulness
Mindfulness, which is being aware of how you feel in the moment, can help you rest better. You can try these mindfulness exercises:
You can also use an app like SoundCloud for free mindfulness exercises.
Activities
Try to do one of the mindfulness activities above every day this week.
You can try different ones to see which one you like best.
Think about what kind of movement or exercise you enjoy. How can you fit it into your week?
You can try one of the ideas above or choose something else that feels right for you.
How Our Mind Affects Our Body
The way we think and feel can affect our health. Stress, worry, or feeling sad can change the way our body works and how we experience illness.
Here are some examples of how our mind affects our body:
· When we are calm, it is easier to concentrate. When we are upset, it is harder.
· Stress can stop us from sleeping well, which can lead to brain fog.
· Pain feels worse when we are sad or having a bad day, but not as bad when we are happy.
What is Stress?
Stress is our body’s way of dealing with danger. Long ago, it helped people escape wild animals, but now it happens for different reasons, like studying, work, or worries about family or money. Some stress can be helpful, like when we have a deadline to meet, but too much stress can make us feel tired and unwell.
Thoughts can cause stress too. If we think something bad might happen, our body reacts as if we are in danger. Over time, too much stress can make us feel exhausted.
Managing Stress with Mindfulness
We can’t always stop stress, but we can change how we react to it. Mindfulness means paying attention to what we feel right now, instead of worrying about the past or future.
Benefits of Mindfulness
· Helps calm the nervous system.
· Brings more awareness of what our body needs.
· Allows us to choose how to respond to a situation
· Helps us enjoy small, happy moments.
· Uses less energy than trying to avoid bad feelings.
Some research shows that mindfulness can reduce stress and improve sleep and may help with coping with persistent pain. Mindfulness may not be suitable for people dealing with very strong emotions or serious mental health problems.
Mindfulness Activities
Here are some activities you can try:
· 3 Minute Breathing Space – A short breathing exercise. https://youtu.be/3oayZww48vA
· Notice 3 Things – Focus on three things around you to help feel present https://youtu.be/UsuY5-K3dXY
Try to make some time to practice these activities every day.
Balancing Our Emotions
We have three emotional systems:
1. Drive system – pushes us to achieve things.
2. Threat system – helps us respond to danger.
3. Soothing system – helps us feel safe and calm.
When we have a long-term condition, the threat and drive systems can take over and we may neglect the soothing system. For example, you might feel anxious when you're in too much pain to work or see friends, or you might push yourself to finish the housework even when you're really tired. If we have too much drive or threat, we can feel overwhelmed. This can make us feel worse.
Doing calming activities, being kind to ourselves, and focusing on things we enjoy can activate the soothing system. This may help reduce sensitivity of the nervous system and pain.
Senses Activity
Try this activity whenever you need to switch on your soothing system.
Write down things you like for each sense. Examples might be the sound of waves, the smell of coffee etc.
Sight - Sound - Touch - Taste - Smell
As you do this, notice how each thing makes you feel. For example, hearing birds sing might remind you of spring and make you feel relaxed.
Try thinking about these things if you need a moment of calm.
Being Kind to Yourself
Being kind to yourself, sometimes known as ‘self -compassion’, also activates the soothing system. Here is a video about being kind to yourself: Watch here.
Some examples of ways to be kind to yourself include
· Talking to yourself as you would talk to a friend
· Making time for something you enjoy · Here is a link to more ways to be kind to yourself: Self-Compassion Practices: Cultivate Inner Peace and Joy - Self-Compassion
Activity: Try to do one kind thing for yourself each day.
Thoughts and Feelings
Thoughts can affect how we feel and behave.
What is a thought?
A thought is an idea or opinion. Thoughts aren’t always true or fair, but they can still affect how we act and feel. This can be a problem when we think negative things about ourselves or our health, because these thoughts can make us feel worse. Knowing that thoughts aren’t facts can help us decide how to respond.
It’s easy to get caught up in our thoughts and act without thinking. This can stop us from acting in a way that matches our values.
Activity
Try the activity below.
What would you think if a friend walked past you without saying hello? How would this make you feel and act?
Now, think of another way to view the same situation. Would that change how you feel or act?
The Hot Cross Bun
To understand more about how thoughts can affect our feelings and actions, we can use the hot cross bun diagram. This video explains more https://youtu.be/Sm-dmGBQ1pg
Activity
Imagine you have to cancel a social event because you are having a flare up of your symptoms. Try to fill out the hot cross bun diagram above by thinking about how you would feel, what you might think, and how you would act in this situation.
Think about what might happen to your values if you focus too much on your thoughts. It can be hard to change what we think, but we can change how we react to those thoughts. For example, you have a choice whether you decide to rebook the social event.
Thinking Styles
We all have ways of thinking that we get used to. Sometimes, these ways of thinking aren’t very helpful.
Here are some examples of thinking styles that people often use.
| Unhelpful Thinking Style | What It Means | Example |
|---|---|---|
| All-or-Nothing Thinking | Seeing things as only good or bad, with no in-between. | "If I don’t get 100% on my test, I’m a total failure!" |
| Overgeneralising | Believing that if something happens once, it will always happen. | "I felt awful when I increased my exercise, it will always be the same." |
| Mind Reading | Thinking you know what others are thinking, even without proof. | "My friend didn’t say hi to me, so she must be mad at me." |
| Catastrophising | Believing something is much worse than it really is. | "My muscles ache, I must be damaging them." |
| Personalisation | Blaming yourself for things that aren’t really your fault. | "The man in the shop was short with me – I must have offended him." |
| Labelling | Calling yourself names instead of looking at the situation as a whole. | "I can't do it – I'm useless." |
| Should Thinking | Telling yourself how things "should" or "must" be, which makes you feel bad. | "I should always be perfect, or I’m not good enough." |
| Filtering | Only noticing the bad things and ignoring the good things. | "I cooked a healthy meal for my children but couldn’t wash up until the next day, I must be a bad parent." |
| Emotional Thinking | Taking a feeling as a fact. | "I feel like a failure so I must be a failure." |
| Fortune-Telling | Acting like you can predict the future, usually in a negative way. | "I just know I’m not going to be able to do it, so I won’t even try." |
This table helps show how some ways of thinking can make us feel worse, even when they’re not really true.
How to Get Unstuck from Unhelpful Thoughts
Sometimes, we get stuck thinking the same way over and over. Sometimes our thoughts can make us feel worse. We can feel stuck in them or believe they are 100% true. But we can change how we respond to our thoughts. Here are some ways to do that:
· Notice your thoughts – Pay attention to what you're thinking.
· Label them – Say to yourself, “I’m having the thought that…” or “here’s a painful thought” or “here’s a judgement” or “here’s the failure story”
· Thank your brain – Your brain is just trying to protect you. Remember that your mind is just doing what it was designed to do – problem solve and avoid danger.
· Ask yourself: Is this thought really true? Is it fair? Is this thought helping me? If not, maybe you can let it go.
· Imagine a friend had this thought. What advice would you give them?
· Try mindfulness. Focus on your breathing instead of your thoughts.
· Say your thoughts out loud (maybe in a silly voice!) or write them down. This can help you see them differently.
· Pay attention to your thinking style. Label it and take a moment before reacting.
· Try the "Leaves on a Stream" meditation. Imagine your thoughts floating away like leaves on a river. Leaves on the stream exercise - Contextual Consulting
Watch this video to understand better how we can get hooked by unhelpful thoughts: Monsters on a Boat
Communication
It can be difficult to ask for help but it can make life easier.
The best way to communicate your needs is calmly, confidently, and respectfully. This is called assertive communication. It helps others understand what you need without arguments.
Tips for Clear Communication
· Use "I" statements. Say "I feel… because…" or "I need…" instead of "You always…"
· Think ahead. Plan what you want to say. It might help to practice or write it down first.
· Pick the right time. Have big conversations when everyone is calm and focused.
· Ask, don’t assume. If you’re unsure what someone is thinking, just ask! And don’t expect people to read your mind—tell them what you need.
· Be clear and confident. Say what you mean without being rude. Keep your body language and voice calm.
· Practice saying "no" without feeling bad. You don’t always need a long excuse. It’s okay to set boundaries.
· Be flexible. Sometimes, working together means finding a middle ground.
· Give compliments! If someone is helpful, let them know. It makes good communication easier.
· Think about your energy. Not every relationship is worth your time. Choose who to focus on.
Activity
Over the next week, pay attention to your thoughts and how you react. Are they helping or making things harder? Try some of the techniques above and see what changes
Pain can affect how we feel and think, and it can make us feel more tired too. Sometimes, pain can make us sad, frustrated, or anxious, and those feelings can make the pain worse.
Here’s how pain affects us in different ways:
- Thoughts and Feelings: Pain can make us feel upset or worried. These feelings can lead us to do things that make the pain worse. For example, we might push ourselves too hard when we feel frustrated, which can make the pain flare up.
- Identity: Pain can change how we see ourselves. It might make us feel like we can’t do things we used to do, like work, spending time with friends, or doing hobbies we enjoy. But it’s important to remember the things that are still important to us, like our values, and try to do things that make us happy even if we can’t do everything we used to. See this video for further explanation: https://www.youtube.com/watch?v=ZUXPqphwp2U
- Mental Health Conditions: Living with pain can make us more likely to feel depressed or anxious, and those feelings can make it harder to feel better.
What You Can Do to Help Your Mental Health:
This is hard for people, and how we think can really affect this. Watching the “Passengers on the bus” video can be a useful way to understand this. You can watch it here: https://youtu.be/yLroVwoPFW8
Another useful strategy to follow is CLANGERS:
C: Connect - with people, nature, community, or yourself. Social Prescribing is a service that can help with this. Social prescribers can help you find activities and groups that can improve your well-being. Your GP can refer to a social prescriber.
L: Learning new things – e.g. watching documentaries, doing puzzles / crosswords, reading, cooking new recipes, learn an instrument.
A: Active – regular movement within your limitations.
N: Notice - who and what is around you, be in the moment without focusing on the past or worrying about the future. This is commonly referred to as mindfulness. You can try a few mindfulness exercises like breathing or body scans to feel better. Here are some videos to try.
G: Give back – we can give our time, buy a small gift for a friend / family member, show gratitude, smile at a stranger, volunteer your time to help your community.
E: Eat well – consider what healthy swaps you could make. See the following link for tips:
https://www.nhs.uk/healthier-families/food-facts/healthier-food-swaps/
R: Rest – you can’t pour from an empty cup, so take time to refill the cup. This could be reading, listening to music, watching tv, sitting in the garden, playing a game, doing mindfulness.
S: Sleep – work on different strategies to maximise your sleep quality – see sleep section later in the programme. Also, think S for Self-compassion: be kind to yourselves.
Here is a video on other tips to help you feel good: BBC - The Social - Learn how to hack your happy hormones
Talking therapy
You can refer yourself for talking therapy on the link below if you are struggling with your mental health. https://notts-talk.co.uk/
They may suggest low intensity therapy with a Psychological Wellbeing Practitioner, or you may be triaged to higher intensity therapy such as CBT. This is a type of therapy that helps you change unhelpful thoughts. It can help you feel better and can be useful if you want to work on specific goals.
ACT (Acceptance & Commitment Therapy): This therapy helps you accept difficult feelings and still move forward. You can learn more about it by watching some videos by a doctor named Russ Harris. Here’s a video that talks about happiness myths: The 3 Happiness Myths
Further Support :
If you ever feel like you’re struggling, here are some places you can reach out to:
- GP or health professional
- Text Notts: A free text support service (Text 85258)
- Samaritans: Call 116 123 for free support
- Turning Point Nottingham: Call 0808 196 3779 for emotional support
Remember, it's okay to ask for help when you're feeling down or struggling with pain. There are people who care about you and want to help you feel better!
In an Emergency
If you ever feel like you want to hurt yourself, it's very important to get help right away. Talk to your GP, the Crisis Team 0808 196 3779 or services like the Samaritans (see above). If you are in immediate danger of harm, call emergency numbers like 111 or 999.
Activity
Look back at the CLANGERS above. Give one or two of them a try this week.
Sleep and pain are closely connected. Sometimes
- Not sleeping well can make your pain worse.
- Having pain can make it hard to sleep.
We know that persistent pain is difficult to treat with medications and so improving sleep is one of the things we can work on to improve pain and quality of life.
Changing your sleep habits can take time, for example a year of steady effort. Many people try something to help their sleep but stop when it doesn’t work right away.
Our plan is to help you understand what might be causing your sleep problems and slowly make changes. These small changes can add up to big improvements.
Why You Might Have Trouble Sleeping
Most sleep problems come from three things:
- Homeostatic Disruption: Things like drinking caffeine or taking naps can confuse your body about when it’s time to sleep.
- Hyperarousal (stress and anxiety): If you’re too worried or thinking too much, your mind stays awake and it’s hard for your body to fall asleep.
- Circadian Disruption (sleep/wake cycle): This happens when your body isn’t used to a regular sleep schedule, for instance falling asleep or waking up at different times every day.
Tips to Help You Sleep Better:
- Don’t force it: If you can’t fall asleep after approximately 20 minutes, get out of bed and do something relaxing for 10 minutes, then try again. It’s important to think of your bed as a place to sleep.
- Avoid blue light: Phones and TVs have blue light that can make your body think it’s still daytime, which keeps you awake. Try to avoid them before bed or put devices onto ‘night mode.’
- Get comfy: Make your bed as comfortable as possible e.g. pillows, blankets, the right temperature (not too hot).
- Write things down: If you can’t stop thinking, try writing your thoughts down before bed, or try mindfulness meditation to calm your mind.
- Take your medicine at the right time: Some medicines, like vitamin D or amitriptyline, should be taken at certain times (generally - take vitamin D in the morning, amitriptyline at night.)
- Get sunlight: Try to get outside in the morning for sunlight, and make sure your curtains block light at night.
Other Helpful Tips
- Everyone is different: Some people are night owls, and some are early birds. Try to find a sleep schedule that works best for you.
- Food and drinks: Caffeine can keep you awake, so don’t drink it after 3 pm. Alcohol might help you fall asleep, but it stops you from sleeping deeply.
- Try new things: You could try listening to calming stories, reading, or using smells like lavender to help you sleep.
Remember: Improving your sleep can take time, but small changes can add up to big improvements!
Further resources
Here are some helpful links for more sleep tips:
- https://www.nhs.uk/every-mind-matters/
- Sleep Stories by Stephen Fry on YouTube
- Michael Mosely’s Program on Sleep
Activity
To help you understand more about your sleep, you can fill out the sleep questionnaire below:
Sleep Questions
Homeostatic Disruption (Things that affect how well you sleep)
- Do you take naps during the day?
- Do you sit or lie down most of the day without moving around much?
- Do you drink things like coffee, tea, soda, or other drinks that have caffeine, or use things like cigarettes or alcohol?
- Do you spend a lot of time in bed when you're not actually sleeping?
Your Body’s Clock (How your body knows when to sleep and wake up)
- Do you wake up at different times each day, even by an hour or more?
- Are you someone who likes staying up late and having trouble waking up early, or the other way around?
Worrying While Sleeping
- Do you spend a lot of time thinking or worrying when you’re trying to sleep?
- Are you worried about your sleep?
- Do you feel like you have to do certain things or follow routines to fall asleep or stay asleep?
- Do you feel stressed, upset, or frustrated when trying to sleep?
- Are you stressed because of school, home, or other things happening in your life?
Do your answers suggest there are any changes you could make in order to improve your sleep? Try these out over the next week but remember, changing your sleep takes time. Don't give up if you don’t notice changes straight away.
How Pain Affects Eating and How You Feel
Pain can make it hard to eat well and take care of your body. When you’re in pain, you might feel tired, stressed, or even sick, which can affect your eating habits. Medications you take might also make you feel nauseous, change how hungry you feel, or affect your stomach and bladder.
When we’re tired, we often eat unhealthy foods that are high in sugar or fat. Nausea can make you not want to eat much at all, and sometimes your mood can affect what you want to eat too. This can make it hard for your body to feel its best. But eating regularly and choosing healthy foods can help your body feel better and reduce stress.
Changing How We Eat Can Feel Hard
Making changes to how we eat when we’re in pain can seem really tough. But it can be helpful to think about small changes you can try, just like you’d suggest to a friend. For example, if you’re tired all the time or your body hurts, cooking can be difficult. People who live with pain have come up with helpful tricks like:
- Cooking big batches of food to store for later
- Using pre-chopped frozen vegetables
- Using kitchen gadgets that make cooking easier (like air fryers or choppers)
If you’re not sure where to start, try searching for “kitchen aids to reduce effort” on the internet for ideas. You can even check out this website for more helpful kitchen tools: Essential Aids.
How Food Affects Mood
What you eat can also affect how you feel. Eating healthy foods can make your mood better because it helps your gut (your stomach and intestines) stay healthy. Your gut is full of tiny bacteria, and these little bacteria can help your brain and body feel good. Eating good food helps keep these bacteria healthy, which helps your whole body work better.
If you have stomach problems, like nausea or an upset stomach, some people find it helpful to drink water regularly or eat smaller meals more often. If eating is really hard, talking to a doctor about seeing a dietitian can help. A dietitian can suggest a special eating plan called the FODMAP diet to help with stomach issues. Here is a link to find out more about a FODMAP diet.
fodmap-gentle-approach-for-irritable-bowel-syndrome_aug24.pdf
What Do Scientists Say?
Doctors and researchers have found that people with long-term pain like fibromyalgia or irritable bowel syndrome often have different gut bacteria than people without pain. Eating better and taking care of your gut might help reduce pain and make you feel better overall. Your gut and your brain are best friends—they talk to each other all the time. This is called the gut-brain axis. If your gut bacteria are not happy, they can send messages to your brain that make pain feel worse. This is called dysbiosis, and it can happen if you eat too much junk food or don’t get enough fibre.
Here are some simple things that can help your gut bugs stay happy—and maybe help your pain too:
- Eat more fibre: Foods like fruits, vegetables, oats, and beans feed your good gut bugs.
- Try fermented foods: Yoghurt, kefir, and sauerkraut have helpful bacteria called probiotics.
- Avoid too much sugar and processed food: These can upset your gut bugs.
- Drink water: It helps your tummy work better.
- Move your body: Walking, dancing, or playing outside helps your gut and your brain.
More about the gut microbiome
Watch the video below to learn more about the gut microbiome.
How the food you eat affects your gut - Shilpa Ravella
Making Healthy Eating Choices
When it comes to what to eat, there’s a lot of advice out there, and it can be confusing. But there’s some easy advice from experts that you can follow:
- Cook food from scratch when you can.
- Eat together with your family or friends when possible.
- Teach children to cook
- Be wary of food adverts and marketing.
Also, the health and supplement industry can be tricky, but a charity called Versus Arthritis has a guide to help you decide if you need any extra supplements. You can read it here: Diet and Nutritional Supplements.
How to Save Money While Eating Well
Food can be expensive, especially now with the cost of living going up. To save money, try cooking in big batches and using frozen or canned foods, which are usually cheaper. You can find lots of budget-friendly recipes online, like these from Jack Monroe: COOKING ON A BOOTSTRAP – by Jack Monroe, bestselling author of 'A Girl Called Jack'
Activity
Eating healthy is really important for your overall health, but when you have pain, it’s easy to forget about taking care of yourself. Eating mindfully and with care can help improve your pain and make you feel better in the long run.
Watch the two videos below and give mindful eating a try this week.
- Mindful eating: https://youtu.be/u1jRaHrpokA
- Mindful eating practice: https://youtu.be/rdb_pC3w-wc
Are there any changes you would like to make to what or how you eat? Can you start to make any of these changes?
Chronic pain is pain that lasts a long time and is hard to treat. Unfortunately, medicines only help a few people and complete relief of pain may not be possible so it's important to have the right expectations.
Goals of Treatment: The main goal is to help people feel better so they can do things they enjoy and feel good emotionally and physically.
Types of pain medication
It is important to understand how the body experiences pain and how different medicines affect specific parts in this process.
There are official guidelines that recommend different medicines for different types of pain.
There are different categories of pain medications. Taking more than one medicine from the same group isn’t usually recommended, so clinicians may advice a switch from one medicine to another, rather than adding new ones.
Taking your medication
If you are switching from one medication to another, this needs to be done under the guidance of a clinician. Often it is done gradually so that your body can gradually get used to the change.
Always follow your clinician’s instructions when taking medicine and contact your GP surgery if you have any issues.
Challenges with medication
Finding the best medicine can take time, and sometimes it can feel like trial and error.
Most pain medications cause side effects, so it is important to consider the risks versus the benefits.
Besides medicine, other treatments like exercises and talking therapies can help some people feel better. These can be used along with medicines.
Opioids
Opioids are strong medicines that work well for short-term pain and pain at the end of life. But they don't help much with long-term pain. Some people feel better when they reduce their medicines, especially painkillers like opioids.
- Some people might get good pain relief from opioids if they take small amounts and not too often. But it's hard to know who these people are when they start taking the medicine.
- Taking high doses of opioids can be harmful and doesn't give extra pain relief.
- If someone is still in pain while taking opioids, the medicine isn't working and should be stopped, even if there are no other treatments available.
- Chronic pain is very complicated. If someone has severe pain and is taking high doses of opioids, it's important to look at all the emotional factors that might be affecting their pain.
Other considerations
- It's important to keep checking if the medicine is still helping and if it should be continued. If you would like to review your pain medications, our pain team offers appointments. Please let us know if you are interested.
- It is also important to know that some pain medications may affect your ability to drive. It is an offence to drive whilst impaired ability due to taking medications (prescribed or not). For further information see: https://www.gov.uk/drug-driving-law
Further resources:
You can read the official pain medicine guidelines here: NICE Chronic Pain Guidelines
This booklet gives a good summary of different types of pain medications, when they may help and possible side effects. Layout 1
Medication Quiz
Have a go at the quiz below to test your knowledge. You will find the answers at the bottom of the page
A flare-up is when your symptoms get worse for a short time. It can make you feel sore, tired, worried, or stressed. It might also stop you from doing things you enjoy. But remember, if you feel more pain, it normally doesn’t mean you have hurt yourself.
What Can Cause a Flare-Up?
Flare-ups can happen for different reasons, and sometimes the cause isn’t clear. Here are some common triggers:
- Doing too much
- Not getting enough rest
- Being sick or having surgery
- Feeling stressed or upset
- Changes in routine
- Changes in weather
- Not sleeping well
- Too much noise or bright lights
How to avoid a flare up
You might not be able to stop flare-ups completely. Planning ahead, pacing and keeping to a routine can stop them happening too often.
How to manage a flare-up
Having a flare up plan can help you cope. Everyone is different, so you need to find what works best for you. Some helpful strategies include:
- Trying not to worry – it can make things worse
- Pacing yourself - resting more and doing less
- Trying some gentle exercise or stretches
- Taking medication
- Using a TENS machine
- Using hot or cold
- Practicing relaxation or mindfulness
- Doing things that calm you
- Using massage
- Asking for help
- Being kind to yourself
- Slowly getting back to normal activity when you feel better
It is OK to feel sad or angry when you have a flare-up. It can be helpful to write your emotions down. Just, remember the flare-up will pass.
Flare-up plans
Having a plan can make flare-ups easier to handle. You can fill out a flare-up plan to help you stay on track when you don’t feel well.
Here is an example of a flare-up plan. You may like to make it personal to you.
|
What can I do during a flareup? |
How can I stick to these ideas during a flare-up? How can I make them easy to do? |
|
Exercise |
Start with half the usual amount. Slowly do more over two weeks.
|
|
Heat |
Use a hot pack 4 times a day. |
|
Mindfulness |
Practise the 5-minute breathing space every hour |
|
Relaxation |
Listen to my relaxation CD twice a day for 15 minutes |
|
Distraction |
Watch my favourite TV programme Read a magazine twice a day for 10 mins |
|
Pacing |
Reduce my activity by about 25% for a week. |
|
Be kind to myself |
Do something nice for myself, like… |
Putting together a flare-up box
A helpful idea is to have a flare-up box ready for when you don’t feel well. This box can have things to help you, like:
- A note to remind yourself that you’ve been through this before and can do it again.
- A hot water bottle to stay warm.
- An exercise sheet with gentle stretches.
- Things to keep you busy, like a good book or a favourite DVD.
Reflecting on your flare-up
Once you start feeling better, it’s good to think about what helped and what didn’t. This way, you can change your plan if needed. You might also want to take some time to write down or think about how you felt.
Here are some questions to help you:
- What might have caused this flare-up?
- What helped me feel better?
- What didn’t work so well?
- Were there any good parts?
- What can I do differently next time?
Further Resources
This link has further information on managing a persistent pain flare-up. Recovering from a persistent pain 'flare' - Living Well with Pain
Local Support Groups
Talking to other people who have persistent pain can help you feel less alone. It can also give you support. You can find links to local groups and organisations for people with persistent pain below.
Fibro Active - Fibromyalgia Support Group Long Eaton
Activity
Complete your own flare up plan using the example above as a guide. You may like to put together your own flare-up box.
Think about your own flare-up triggers. Can you make any changes to limit the chance of a flare-up happening?
Moving forwards
Congratulations! You have reached the end of our online pain management programme. We hope you have found the information and activities helpful. Your clinician will be happy to answer any questions you may have.
Keep trying the ideas from this programme - they can help you enjoy life even with pain. But remember, change takes time. Above all, be kind to yourself!

